
Shaker Q. M. Nawasreh, Mohammad Hassan Ennab, Emad Rababah
22-8-2018
ABSTRACT
This study explores the radiation safety culture traits within the Nuclear Medicine Department at Al Hussain Medical Center, focusing on staff commitment to ten key traits: individual responsibility, questioning attitude, effective safety communication, leadership responsibility, decision-making, respectful work environment, continuous learning, problem identification and resolution, environment for raising concerns, and work processes. Data was gathered from a diverse group of professionals, including technicians, nurses, physicians, and physicists. While the department demonstrates a strong foundation in safety culture, areas such as decision-making processes and resource availability require improvement.
The study highlights the crucial role of leadership in creating a safety-conscious environment and underscores the importance of individual responsibility in maintaining safety standards. It concludes that, although a solid radiation safety culture exists, continuous efforts are needed to improve decision-making clarity, foster open communication, and ensure consistent training.
These findings establish a baseline for future evaluations and provide a framework for developing targeted strategies to support ongoing improvement and reinforce safety culture within nuclear medicine.
Introduction
In the field of nuclear medicine, ensuring radiation safety is paramount to safeguarding the health and well-being of both healthcare professionals and patients. The growing use of radioactive materials in diagnostic and therapeutic procedures underscores the need for a strong safety culture within medical institutions. A well-developed radiation safety culture reflects a shared commitment to prioritizing safety above competing objectives, creating an environment where safety considerations are embedded in all aspects of operation.
Therefore, it is essential and fundamental to continue studying and monitoring the ability of nuclear medicine professionals to implement radiation safety standards and to enhance these capabilities.
Additionally, learning from experiences, consulting and following the accredited International Organizations publications, and gaining insights from them are crucial for sustaining radiation safety programs within institutions and departments that utilize medical radioactive isotopes Primarily Nuclear Medicine Centers.
Therefore, this study examined the ability of nuclear medicine professionals to apply, adhere to, and consistently learn these standards correctly and sustainably, aiming to assess the level of compliance with the standards.
Objectives
The primary objective of this study is to assess the level of radiation safety culture among the staff at Al Hussain Medical Center, with a particular focus on their awareness of safety principles and their adherence to established safety practices. The study aims to:
1. Investigate potential radiation hazards in the nuclear medicine department and establish appropriate procedures for managing incidents or potential exposures.
2.Evaluate the staff’s understanding of essential radiation safety culture traits, such as: individual responsibility, effective communication, leadership commitment, and continuous learning.
3.Propose strategies and policies to enhance the overall radiation safety culture, focusing on leadership engagement and staff participation in safety practices.
Literature review
The importance of radiation safety in nuclear medicine cannot be overstated, as it plays a crucial role in protecting both healthcare workers and patients from unnecessary exposure. Several key works provide valuable insights into the implementation and enhancement of radiation safety standards in nuclear medicine.
1. Radiation Safety and Accidental Radiation Exposures in Nuclear Medicine This article explores the various types of radiation exposures encountered by nuclear medicine staff, emphasizing the need for effective dose constraints and strict safety protocols. It highlights practical measures that mitigate the risks associated with radiation exposure in clinical settings, offering concrete guidance for staff working with radiopharmaceuticals and other radioactive materials. This article serves as a critical resource for understanding the direct application of safety measures in nuclear medicine departments.
2. Applying Radiation Safety Standards in Nuclear Medicine (IAEA) Published by the International Atomic Energy Agency (IAEA), this report outlines the International Basic Safety Standards (BSS) for radiation protection. It offers a comprehensive overview of the legal responsibilities, safe working procedures, and the importance of regular training and updates for nuclear medicine personnel. By establishing clear guidelines, the BSS ensures that facilities maintain a high level of safety and compliance with international standards. This document emphasizes the necessity of continuous education to reinforce safety culture in nuclear medicine departments.
3. Radiation Protection in Nuclear Medicine: Best Practice This paper outlines the best practices for radiation protection, particularly focusing on the safe administration of radiopharmaceuticals. It underscores the importance of ongoing staff training and the consistent implementation of international safety standards to safeguard both patients and personnel. The paper is instrumental in detailing protocols that minimize radiation exposure while ensuring effective medical treatment.
4. Human Health Campus – Radiation Protection of Workers and the Public in Nuclear Medicine This article addresses the principles of radiation protection specifically for workers and the public within nuclear medicine settings. It covers essential aspects such as dose limits, facility design, access control, and safe operational procedures. These elements are critical in ensuring that occupational personnel and the public remain protected from unnecessary radiation exposure. The article’s focus on facility design and dose limits provides a foundation for departments to implement structural safety improvements in their operations.
5. Radiation Protection Culture, Communication, and Context This paper delves into the complexities of fostering a radiation protection culture within organizations. It highlights the role of effective communication and the context in which safety practices are applied, offering insights into how cultural and organizational factors influence radiation safety. By emphasizing the importance of open communication channels and a proactive approach to safety, the paper advocates for a well-rounded safety culture that permeates all levels of an organization.
Some gaps in the current literature:
1. Practical outcomes:
• While most references emphasize the importance of adherence to radiation safety standards, specific data on how well nuclear medicine staff adhere to these standards in practice are limited.
• Studies such as “Radiation Safety and Accidental Radiation Exposures in Nuclear Medicine” focus on general protocols rather than detailed compliance statistics or observational data.
2. Impact of Behavior on Personal Radiation Safety:
The references do not offer a comprehensive evaluation of how correct and incorrect behaviors affect personal radiation safety. The need for detailed behavioral studies and their correlation with safety outcomes is evident, as highlighted in References 1 and 4.
4.Expected outcomes and impact
The study aimed to improve the understanding of nuclear medicine staff’s awareness and adherence to radiation safety standards. It sought to identify key areas of weakness in current safety practices and traits, offering insights into the effectiveness of existing training programs and highlighting critical topics for future training initiatives.
The study also provided recommendations for improving radiation safety protocols and staff education, ultimately developing actionable strategies to strengthen overall radiation protection and safety culture within the organization.
5.Study Introduction
This research aimed to assess the radiation safety culture at the Nuclear Medicine Department in King Hussein Medical City, Jordan, using a questionnaire that was distributed over 65 department’s staff from various specialties. The questionnaire addressed various demographic aspects of the participants, including age, job title, experience, and educational level. It also covered key traits of radiation safety culture, such as individual responsibility, the encouragement of a questioning attitude, effective communication regarding safety, leadership commitment to safety, decision-making processes concerning safety, a respectful work environment, continuous learning, problem identification and resolution, a supportive environment for raising concerns, and the integration of safety into daily work processes. The questionnaire was designed to gather comprehensive data that reflected the staff’s adherence to radiation safety traits and their efforts to promote a strong safety culture.
Why Radiation safety in nuclear medicine is important?
Radiation safety in nuclear medicine is vital to protect patients, healthcare workers, and the public from unnecessary radiation exposure, which can lead to severe health risks. Ensuring that safety protocols are followed reduces the likelihood of radiation-related accidents, while optimizing dose administration maximizes diagnostic and therapeutic benefits without compromising health. Adherence to international safety standards, such as those from the IAEA, fosters a culture of responsibility and continuous improvement. Effective communication of risks and safety procedures further enhances trust and compliance, making radiation safety an essential aspect of delivering high-quality medical care:(iaea_webinar_radiation_…)(OD52_TheFutureOfRP_Wilk…)(Pub1578_web-57265295)(s00259-024-06633-w).
6.Proposed Methodology
The study employs a questionnaire, designed in alignment with the previously discussed objectives and identified gaps which were identified through a review of existing literature and practices related to radiation safety in nuclear medicine, focusing on the areas where current research or protocols lacked detailed insights to focus on several specific areas like:
• Adherence to Standards as the need for more detailed, practice-oriented data on compliance was evident.
• Behavioral Impact: as behavioral studies and their correlation with safety outcomes were identified as a gap.
• Practical Application of Safety Protocols: This lack of specific, applied insights created a gap in understanding how protocols were being implemented and followed on the ground.
A Set of 30 questions (annex -1) prepared, targeted questions nuclear medicine staff at Al Hussein Nuclear Medicine Department. The questions were aimed to assess the staff’s understanding of radiation safety traits, evaluate their current practices, and identify areas for potential improvement.
The questionnaire distributed within a defined timeframe and will address the following traits:
These traits, derived from the ‘Radiation Safety Culture Trait Talks Handbook ‘ are intended to assess the radiation safety culture within any radiology department.
These traits promote a safe, accountable environment where every team member actively prioritizes safety. Key traits include individual responsibility, effective communication, and leadership commitment, which ensure clarity, accountability, and open dialogue. Continuous learning and a questioning attitude prevent complacency and adapt practices to evolving safety needs. Effective decision-making and structured work processes ensure consistent safety standards, while a respectful environment allows concerns to be raised freely, reinforcing a collaborative and proactive safety culture.
Radiation Safety Culture Traits include :
1.Individual Responsibility.
2.Effective Safety Communication.
3.Questioning Attitude.
4.Leadership Responsibility.
5.Decision Making.
6.Respectful Work Environment.
7.Continuous Learning.
8.Problem Identification and Resolution.
9.Environment for Raising Concerns.
10.Work Processes.
The collected data will be analyzed using descriptive statistics to summarize the responses and inferential statistics to identify significant patterns and correlations.
Our statistical analysis primarily focused on the following terms to describe the resulting data: mean, standard deviation, frequency, percentage, and Chi-square tests.
7.Results of the Questioner
Statistical Analysis Results:
The survey was distributed to 62 staff members in the Nuclear Medicine Department, with 62 completed responses collected. The participants ranged from technicians, physicists, and other nuclear medicine professionals as follows :
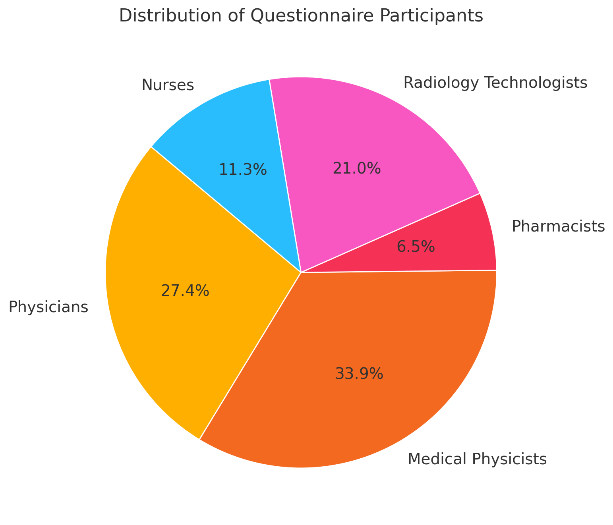
The questionnaire participants were categorized as follows: 17 physicians, 21 medical physicists, 4 pharmacists, 13 radiology technologists, and 7 nurses, with varying levels of experience and education .
Most respondents displayed a positive attitude toward radiation safety practices, with high levels of agreement across key traits, such as individual responsibility, effective communication, and leadership commitment:
•Individual Responsibility: 90% of respondents agreed or strongly agreed that they take personal responsibility for radiation safety in their daily tasks.
•Questioning Attitude: 60% of staff members reported that they are encouraged to question procedures and practices that may impact radiation safety.
•Leadership Commitment: 80% of respondents agreed or strongly agreed that leadership in their department demonstrates a commitment to radiation safety.
•Continuous Learning: The majority of respondents, 85%, agreed that ongoing training and education on radiation safety are integral parts of their work environment.
•Work Processes: 65% of staff agreed that work processes are regularly reviewed and updated to enhance radiation safety, though 10% indicated disagreement, highlighting an area for improvement.
While the general consensus was positive, a few areas require attention. For instance, only 70% of respondents felt confident in decision-making processes related to radiation safety, suggesting a need for more clarity and resource availability in this domain.
Additionally, a small portion of the staff (around 15%) expressed concerns about the frequency of updates to safety procedures and access to continuous learning resources.
The survey analysis highlights key traits within the Nuclear Medicine Department at Al Hussain Medical Center, with staff members displaying generally positive attitudes towards radiation safety. The mean scores for each trait suggest a strong sense of individual responsibility (Mean = 4.0, SD = 0.72) and a questioning attitude (Mean = 4.11, SD = 0.68). Effective safety communication received a slightly lower mean score (Mean = 3.84, SD = 0.88), indicating room for enhanced clarity and frequency of communication. Leadership commitment was rated with a mean of 3.82 (SD = 0.85), reflecting positive engagement with safety priorities, although variability suggests differing perceptions among staff.
Decision-making processes were moderately rated (Mean = 3.89, SD = 0.77), with a need for more consistency and support across roles. Respectful work environment and continuous learning were both positively rated (Means = 3.89, 3.86; SDs = 0.70, 0.72, respectively), with staff affirming a collaborative environment and the importance of ongoing safety education. The environment for raising concerns received one of the highest mean scores (Mean = 3.90, SD = 0.67), while work processes also showed solid engagement (Mean = 3.81, SD = 0.79), though some responses suggest variability in how well these are reviewed and updated.
Overall, these statistics illustrate a foundational commitment to radiation safety culture, with certain areas showing variability that may benefit from targeted improvements in consistency and resources to support decision-making and communication.
Conclusion
This study has assessed the radiation safety culture at the Nuclear Medicine Department of Al Hussain Medical Canter, focusing on staff adherence to essential safety traits such as individual responsibility, leadership commitment, effective communication, and continuous learning. The survey results indicate a strong foundation in radiation safety culture, with high levels of personal responsibility and leadership engagement. Staff members generally understand the importance of radiation safety, and their attitudes reflect a commitment to upholding safety standards.
However, areas for improvement were identified, particularly in decision-making processes and resource availability. The study highlighted that staff members sometimes experience ambiguity in decision-making, which can lead to inconsistencies in radiation safety practices. Furthermore, limitations in resources, such as updated safety tools and materials, hinder the consistent application of best practices. These areas should be addressed to ensure that all staff members have the necessary clarity and resources to follow radiation safety protocols effectively.
In conclusion, while Al Hussain Medical Canter demonstrates a commendable commitment to radiation safety, continuous efforts are needed to enhance decision-making protocols, improve resource availability, and ensure consistent staff engagement with
evolving safety standards. Strengthening these areas will further solidify the safety culture and protect both patients and staff from unnecessary radiation exposure.
9.Future Suggestions
To further improve the radiation safety culture in the department, the following recommendations are proposed:
1.Refinement of Decision-Making Protocols: There is a need to develop clearer and more structured decision-making processes related to radiation safety. This can be achieved by creating detailed guidelines and flowcharts that staff can refer to during critical situations. Regular simulations and drills could help familiarize staff with these protocols and improve their response times in emergencies.
2.Enhanced Resource Availability: Ensuring that staff members have access to the most up-to-date safety tools and resources is crucial. This could involve updating radiation monitoring devices, increasing access to protective equipment, and maintaining an adequate supply of training materials. Additionally, a regular review process should be established to identify resource gaps and address them promptly.
3.Continuous Training and Education: While the survey indicated positive feedback on continuous learning, it is essential to provide ongoing training programs that reflect the latest developments in radiation safety. Regular workshops and refresher courses, particularly focusing on emerging technologies and updated international standards, should be prioritized. Collaborating with international agencies such as the IAEA could ensure that training materials remain relevant and comprehensive.
16
4.Improving Safety Communication: Effective communication is key to maintaining a strong safety culture. Introducing more frequent and structured safety briefings, along with open forums for staff to voice concerns, would foster transparency and improve the flow of information. Moreover, promoting a questioning attitude where staff are encouraged to raise issues without fear of repercussion will further enhance the department’s overall safety practices.
5.Routine Safety Audits: Conducting regular internal audits to assess compliance with safety standards and protocols will ensure that the department continues to uphold a high standard of radiation safety. These audits should evaluate both the technical aspects of radiation safety as well as behavioural adherence to safety practices, ensuring that improvements are data-driven and targeted.
By addressing these areas, the Nuclear Medicine Department at Al Hussain Medical Canter can build on its current strengths and foster an environment of continuous improvement in radiation safety culture.
BIBLIOGRAPHY
1.McCardle, J., & Chester, D. (2001). “Measuring an Asynchronous Processor’s Power and Noise.” Synopsys User Group Conference (SNUG), Boston.
2.Seitz, C. L. (1980). “System Timing.” In Introduction to VLSI Systems (pp. 218–262). Addison-Wesley.
3.International Atomic Energy Agency (IAEA). (n.d.). Radiation Protection of Workers and the Public in Nuclear Medicine. Retrieved from IAEA Human Health Campus.
4.ACI Committee 440. (2001). Guide for the Design and Construction of Concrete Reinforced with FRP Bars (440.1R-01). American Concrete Institute, Farmington Hills, Michigan.
5.Canny, J. (1986). “A Computational Approach to Edge Detection.” IEEE Transactions on Pattern Analysis and Machine Intelligence (PAMI), 10, 679-698.
6.Radiation Safety and Accidental Radiation Exposures in Nuclear Medicine. (n.d.). Journal of Nuclear Medicine Technology, (journal issue and volume if available).
7.International Atomic Energy Agency (IAEA). (n.d.). Applying Radiation Safety Standards in Nuclear Medicine. Retrieved from IAEA.org.
8.IAEA. (n.d.). International Basic Safety Standards (BSS) for Radiation Protection.
9.Human Health Campus – Radiation Protection Culture, Communication, and Context. (n.d.). IAEA.